Paper Review: the Babylon Chatbot
June 29, 2018 § 2 Comments
[For convenience I collect here and slightly rearrange and update my Twitter review of a recent paper comparing the performance of the Babylon chatbot against human doctors. As ever my purpose is to focus on the scientific quality of the paper, identify design weaknesses, and suggest improvements in future studies.]
Here is my peer review of the Babylon chatbot as described in the conference paper at https://marketing-assets.babylonhealth.com/press/BabylonJune2018Paper_Version1.4.2.pdf
Please feel free to correct any misunderstandings I have of the evaluation in the tweets that follow.
To begin, the Babylon engine is a Bayesian reasoner. That’s cool. Not sure if it qualifies as AI.
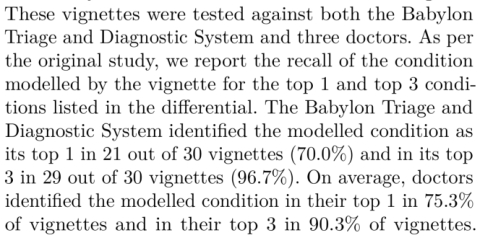
The evaluation uses artificial patient vignettes which are presented in a structured format to human GPs or a Babylon operator. So the encounter is not naturalistic. It doesn’t test Babylon in front of real patients.
In the vignettes, patients were played by GPs, some of whom were employed by Babylon. So they might know how Babylon liked information to be presented and unintentionally advantaged it. Using independent actors, or ideally real patients, would have had more ecological validity.
A human is part of the Babylon intervention because a human has to translate the presented vignette and enter it into Babylon. In other words, the human heard information that they then translated into terminology Babylon recognises. The impact of this human is not explicitly measured. For example, rather than being a ‘mere’ translator, the human may occasionaly have had to make clinical inferences to match case data to Babylon capabilty. The knowledge to do that would thus be be external to Babylon and yet contribute to its performance, if true.
The vignettes were designed to test know capabilities of the system. Independently created vignettes exploring other diagnoses would likely have resulted in a much poorer performance. This tests Babylon on what it knows not what it might find ‘in the wild’.
It seems the presentation of information was in the OSCE format, which is artificial and not how patients might present. So there was no real testing of consultation and listening skills that would be needed to manage a real world patient presentation.
Babylon is a Bayesian reasoner but no information was presented on the ‘tuning’ of priors required to get this result. This makes replication hard. A better paper would provide the diagnostic models to allow independent validation.
The quality of differential diagnoses by humans and Babylon was assessed by one independent individual. In addition two Babylon employees also rated differential diagnosis quality. Good research practice is to use multiple independent assessors and measure inter-rater reliability.
The safety assessment has the same flaw. Only 1 independent assessor was used and no inter-rater reliability measures are presented when several in-house assessors are added. Non-independent assessors bring a risk of bias.
To give some further evaluation, additional vignettes are used, based on MRCGP tests. However any vignettes outside of the Babylon system’s capability were excluded. They only tested Babylon on vignettes it had a chance to get right.
So, whilst it might be ok to allow Babylon to only answer questions that it is good at for limited testing, the humans did not have a reciprocal right to exclude vignettes they were not good at. This is fundamental bias in the evaluation design.
A better evaluation model would have been to draw a random subset of cases and present them to both GPs and Babylon.
No statistical testing is done to check if the differences reported are likely due to chance variation. A statistically rigorous study would estimate the likely effect size and use that to determine the sample size needed to detect a difference between machine and human.
For the first evaluation study, methods tells us “The study was conducted in four rounds over consecutive days. In each round, there were up to four “patients” and four doctors.” That should mean each doctor and Babylon should have seen “up to” 16 cases.
Table 1 shows Babylon used on 100 vignettes and doctors typically saw about 50. This makes no sense. Possibly they lump in the 30 Semigran cases reported separately but that still does not add up. Further as the methods for Semigran were different they cannot be added in any case.
There is a problem with Doctor B who completes 78 vignettes. The others do about 50. Further looking at Table 1 and Fig 1 Doctor B is an outlier, performing far worse than the others diagnostically. This unbalanced design may mean average doctor performance is penalised by Doctor B or the additional cases they saw.
Good research practice is to report who study subjects are and how they were recruited. All we know is that these were locum GPs paid to do the study. We should be told their age, experience and level of training, perhaps where they were trained, whether they were independent or had a prior link to the researchers doing the study etc. We would like to understand if B was somehow “different” because their performance certainly was.
Removing B from the data set and recalculating results shows humans beating Babylon on every measure in Table 1.
With such a small sample size of doctors, the results are thus very sensitive to each individual case and doctor, and adding or removing a doctor can change the outcomes substantially. That is why we need statistical testing.
There is also a Babylon problem. It sees on average about twice as many cases as the doctors. As we have no rule provided for how the additional cases seen by Babylon were selected, there is a risk of selection bias eg what if by chance the ‘easy’ cases were only seen by Babylon?
A better study design would allocate each subject exactly the same cases, to allow meaningful and direct performance comparison. To avoid known biases associated with presentation order of cases, case allocation should be random for each subject.
For the MRCGP questions Babylon’s diagnostic accuracy is measured by its ability to identify a disease within its top 3 differential diagnoses. It identified the right diagnosis in its top 3 in 75% of 36 MRCGP CSA vignettes, and 87% of 15 AKT vignettes.
For the MRCGP questions we are not given Babylon’s performance when the measure is the top differential. Media reports compare Babylon against historical MRCGP human results. One assumes humans had to produce the correct diagnosis, and were not asked for a top 3 differential.
There is huge significance clinically in putting a disease in your top few differential diagnoses and the top one you elect to investigate. It also is an unfair comparison if Babylon is rated by a top 3 differential and humans by a top 1. Clarity on this aspect would be valuable.
In closing, we are only ever given one clear head to head comparison between humans and Babylon, and that is on the 30 Semigran cases. Humans outperform Babylon when the measure is the top diagnosis. Even here though, there is no statistical testing.
So, in summary, this is a very preliminary and artificial test of a Bayesian reasoner on cases for which it has already been trained.
In machine learning this would be roughly equivalent to in-sample reporting of performance on the data used to develop the algorithm. Good practice is to report out of sample performance on previously unseen cases.
The results are confounded by artificial conditions and use of few and non-independent assessors.
There is lack of clarity in the way data are analysed and there are numerous risks of bias.
Critically, no statistical testing is performed to tell us whether any of the differences seen mean anything. Further, the small sample size of GPs tested likely means it would be unlikely that this study was adequately powered to see any difference, if it does exist.
So, it is fantastic that Babylon has undertaken this evaluation, and has sought to present it in public via this conference paper. They are to be applauded for that. One of the benefits of going public is that we can now provide feedback on the study’s strength and weaknesses.
Journal Review: Watson for Oncology in Breast Cancer
March 9, 2018 § Leave a comment
How should we interpret research reporting the performance of #AI in clinical practice?
[This blog collects together in one place a twitter review published 9 March 2018 at https://twitter.com/EnricoCoiera/status/971886744101515265 ]
Today we are reading “Watson for Oncology and breast cancer treatment recommendations: agreement with an expert multidisciplinary tumor board” that has just appeared in the Annals of Oncology.
https://academic.oup.com/annonc/article/29/2/418/4781689
This paper studies the degree of agreement or “concordance” between Watson for Oncology (WFO) and an expert panel of clinicians on a ’tumor board’. It reports an impressive 93% concordance between human experts and WFO when recommending treatment for breast cancer.
Unfortunately the paper is not open access but you can read the abstract. I’d suggest reading the paper before you read further into this thread. My question to you: Do the paper’s methods allow us to have confidence in the impressive headline result?
We should begin by congratulating the authors on completing a substantial piece of work in an important area. What follows is the ‘review’ I would have written if the journal had asked me. It is not a critique of individuals or technology and it is presented for educational purposes.
Should be believe the results are valid, and secondly do we believe that they generalizable to other places or systems? To answer this we need to examine the quality of the study, the quality of the data analysis, and the accuracy of the conclusions drawn from the analysis.
I like to tease apart the research methods section using PICO headings – Population, Intervention, Comparator, Outcome.
(P)opulation. 638 breast cancer patients presented between 2014-16 at a single institution. However the study excluded patients with colloid, adenocystic, tubular, or secretory breast cancer “since WFO was not trained to offer treatment recommendations for these tumor types”.
So we have our first issue. We are not told how representative this population is of the expected distribution of breast cancer cases at the hospital or in the general population. We need to know if these 3 study years were somehow skewed by abnormal presentations.
We also need to know if this hospital’s case-mix is normal or somehow different to that in others. Its critical because any claim for the results here to generalize elsewhere depends on how representative the population is.
Also, what do we think of the phrase “since WFO was not trained to offer treatment recommendations for these tumor types”? It means that irrespective of how good the research methods are, the result will not necessarily hold for *all breast cancer cases”
All they can claim is that any result holds for this subset of breast cancers . We have no evidence presented to suggest that performance would be the same on the excluded cancers. Unfortunately the abstract and paper results section do not include this very important caveat.
(I)ntervention. I’m looking for a clear description of the intervention to understand 1/ Could someone replicate this intervention independently to validate the results? 2/ What exactly was done so that we can connect cause (intervention) with effect (the outcomes)?
WFO is the intervention. But it is never explicitly described. For any digital intervention, even if you don’t tell me what is inside the black box, I need 2 things: 1/ Describe exactly the INPUT into the system and 2/ describe exactly the OUTPUT from the system.
This paper unfortunately does neither. There is no example of how a cancer case is encoded for WFO to interpret, nor is there is an example of a WFO recommendation that humans need to read.
So the intervention is not reported in enough detail for independent replication, we do not have enough detail to understand the causal mechanism tested, and we don’t know if biases are hidden in the intervention. This makes it hard to judge study validity or generalizability
Digging into an online appendix, we do discover some details about input, and WFO mechanism. It appears WFO is input a feature vector:
It also appears that vector is then input to an unspecified machine learning engine that presumably associates disease vectors with treatments.
So, for all the discussion of WFO as a text-processing machine, at its heart might be a statistical classification engine. It’s a pity we don’t know any more, and it’s a pity we don’t know how much human labour is hidden in preparing feature vectors and training cases.
But there is enough detail in the online appendix to get a feeling about what was in general done. They really should have been much more explicit and included the input feature vector, and output treatment recommendation description in the main paper.
But was WFO really the only intervention? No. there was also a human intervention that needs to be accounted for and it might very well have been responsible for some % of the results.
The Methods reports that two humans (trained senior oncology fellows) entered the data manually into WFO. They read the cases, identified the data that matched the input features, and then decided the scores for each feature. What does this mean?
Firstly, there was no testing of inter-rater reliability. We don’t know if the two humans coded the same cases in the same way. Normally a kappa statistic is provided to measure the degree of agreement between humans and allow us to get a sense for how replicable what they did was.
For example, a low kappa means that agreement is low and that therefore any results are less likely to replicate in a future study. We really need that kappa to trust the methods were robust.
If humans are pre-digesting data for WFO how much of WFO’s performance is due to the way humans seek, identify and synthesize data? We don’t know. One might argue that the hard information detection and analysis task is done by humans and the easier classification task by WFO.
So far we have got to the point where the papers’ results are not that WFO had a 93% concordance with human experts, but rather that, when humans from a single institution read cancer cases from that institution, and extract data specifically in the way that WFO needs it, and also when a certain group of breast cancers are excluded, then concordance is 93%. That is quite a list of caveats already.
(C)ompartor: The treatments recommended by WFO are compared to the consensus recommendations of a human group of experts. The authors rightly noted that treatments might have changed between the time the humans recommended a treatment and WFO gave its recommendation. So they calculate concordance *twice*.
The first comparison is between treatment recommendations of the tumor board and WFO. The second is not so straightforward. All the cases in the first comparison for which there was no human/WFO agreement were taken back to the humans, who were asked if their opinion had changed since they last considered the case. A new comparison was then made between this subset of cases and WFO, and the 93% figure comes from this 2nd comparison.
We now have a new problem. You know you are at risk of introducing bias in a study if you do something to one group that is different to what you do to the other groups, but still pool the results. In this case, the tumor board was asked to re-consider some cases but not others.
The reason for not looking at cases for which there had been original agreement could only be that we can safely assume that the tumor board’s views would not have changed over time. The problem is that we cannot safely assume that. There is every reason to believe that for some of these cases, the board would have changed its view.
As a result, the only outcomes possible at the second comparisons are either no change in concordance or improvement in concordance. The system is inadvertently ’rigged’ to prevent us discovering there was a decrease in concordance over time because the cases that might show a decrease are excluded from measurement.
From my perspective as a reviewer that means I can’t trust the data in the second comparison because of a high risk of bias. The experiment would need to be re-run allowing all cases to be reconsidered. So, if we look at the WFO concordance rate at first comparison, which is now all I think we reasonably can look at, it drops from 93% to 73% (Table 2).
(O)utcome: The outcome of concordance is a process not a clinical outcome. That means that it measures a step in a pathway, but tells us nothing about what might have happened to a patient at the end of the pathway. To do that we would need some sort of conversion rate.
For example if we knew for x% of cases in which WFO suggested something humans had not considered, that humans would change their mind, this would allow us to gauge how important concordance was in shaping human decision making. Ideally we would like to know a ‘number needed to treat’ i.e. how many patients need to have their case considered by WFO for 1 patient to materially benefit e.g. live rather than die.
So whilst process outcomes are great early stepping-stones in assessing clinical interventions, they really cannot tell us much about eventual real world impact. At best they are a technical checkpoint as we gather evidence that a major clinical trial is worth doing.
In this paper, concordance is defined as a tricky composite variable. Concordance = all those cases for which WFO’s *recommendation* agreed with the human recommendation + all those cases in which the human recommendation appeared in a secondary WFO list of *for consideration* treatments.
The very first question I now want to know is ‘how often did human and WFO actually AGREE on a single treatment?” Data from the first human-WFO comparison point indicates that there was agreement on the *recommended* treatment in 46% of cases. That is a very different number to 93% or even 73%.
What is the problem with including the secondary ‘for consideration’ recommendations from WFO? In principle nothing, as we are at this point only measuring process not outcomes, but it might need to be measured in a very different way than it is at present for the true performance to be clear.
Our problem is that if we match a human recommended treatment to a WFO recommendation it is a 1:1 comparison. If we match human recommended to WFO ‘for consideration’ it is 1:x. Indeed from the paper I don’t know what x is. How long is this additional list of ‘for consideration’ treatments. 2,5,10? You can see the problem. If WFO just listed out the next 10 most likely treatments, there is a good chance the human recommended treatment might appear somewhere in the list. If it had listed just 2 that would be more impressive.
In information retrieval, there are metrics that deal with this type of data, and they might have been used here. You could for example report the median rank at which WFO ‘for considerations’ matched human recommendations. IN other words, rather than treating it as a binary yes/no we would better assess performance by measuring where in the list the correct recommendation is made.
Now lets us turn to the results proper. I have already explained my concerns about the headline results around concordance.
Interestingly concordance is reportedly higher for stage II and III disease and lower for stage 1 and 1V. That is interesting, but odd to me. Why would this be the case? Well, this study was not designed to test for whether concordance changes with stage – this is a post-hoc analysis. To do such a study, we would likely have had to have seek equal samples of each stage of disease. Looking at the data, stage I cases are significantly underrepresented compared to other stages. So interesting, but treat with caution.
There are other post-hoc analyses of receptor status and age and the relationship with concordance. Again this is interesting but post-hoc so treat it with caution.
Interestingly concordance decreased with age – and that might have something to do with external factors like co-morbidity starting to affect treatment recommendations. Humans might for example, reason that aggressive treatment may not make sense to a cancer patient with other illnesses and at a certain age. The best practice encoded in WFO might not take such preferences and nuances into account.
Limitations: The authors do a very good job overall in identifying many, but not all, of the issues I raise above. Despite these identified limitations, which I think are significant, they still see WFO’s producing a “high degree of agreement’ with humans. I don’t think the data yet supports that conclusion.
Conclusions: The authors conclude by suggest that as a result of this study WFO might be useful for centers with limited breast cancer resources. The evidence in this study doesn’t yet support such a conclusion. We have some data on concordance, but no data on how concordance affects human decisions, and no data on how changed decisions affects patient outcomes. Those two giant evidence gaps mean it might be a while before we safely trial WFO in real life.
So, in summary, my takeaway is that WFO generated the same treatment recommendation as humans for a subset of breast cancers at a single institution in 46% of cases. I am unclear how much influence human input had in presenting data to WFO, and there is a chance the performance might have been worse without human help (e.g. if WFO did its own text processing).
I look forward to hearing more about WFO and similar systems in other studies, and hope this review can help in framing future study designs. I welcome comments on this review.
[Note: There is rich commentary associated with the original Twitter thread, so it is worth reading if you wish to see additional issues and suggestions from the research community.]